Cs Slot
The Federation of State Medical Boards (FSMB) and NBME, co-sponsors of the United States Medical Licensing Examination® (USMLE®), have discontinued work to relaunch a modified Step 2 Clinical Skills examination (Step 2 CS). See full announcement and podcast for more information.
Overview
Were Sam and Chris. A fun loving couple that enjoys playing slot machines together at the casino and catching big wins on video! Join us as we travel to different casinos, chasing good times. Ai obligatia de a pune un link cu orele jucate, pana nu postezi acel link, si raspunzi aiure, ai Contra. Edit: Felicitari ca ai pus orele jucate dar tot Contra ramane, deoarece ai 3 ore pe server iar cerintele sunt.
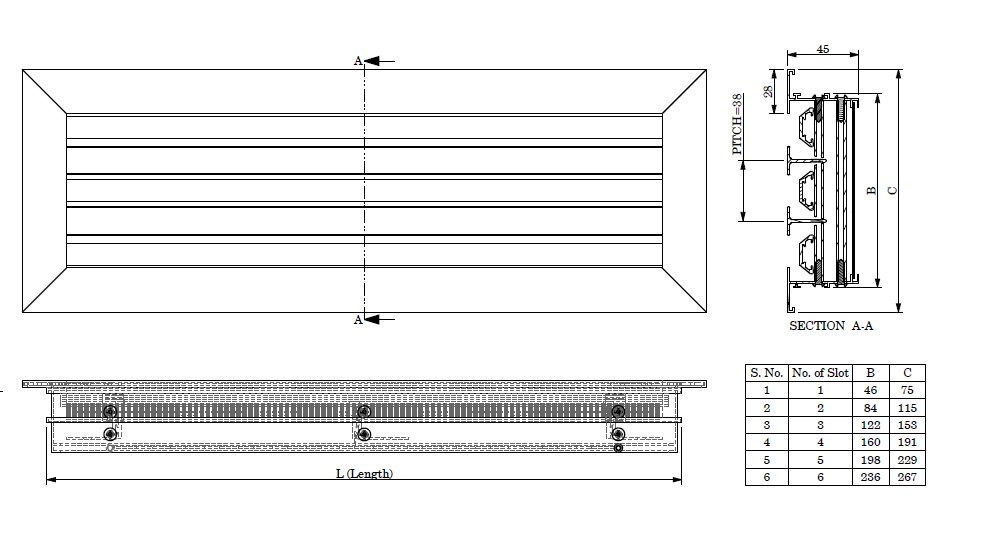
The Waterloo small format continuous slot diffuser series CS has for many years set the industry standard in terms of highest aerodynamic and acoustic performance. The CS range is ideally suited to variable volume applications due to its excellent low flow rate air diffusion characteristics and high air handling capacity. Csbd community in partnership with krond solutions: counter strike 1.6 servers - 13 euro BUY KROND SERVER HOSTING - 13EUR In partnership with Krond Solutions we offer you the CounterStrike 1.6 servers, 32 slots, 1000fps for only 13 EURO.
Step 2 of the USMLE assesses the ability of examinees to apply medical knowledge, skills, and understanding of clinical science essential for the provision of patient care under supervision, and includes emphasis on health promotion and disease prevention. Step 2 ensures that due attention is devoted to the principles of clinical sciences and basic patient-centered skills that provide the foundation for the safe and effective practice of medicine.
Step 2 CS uses standardized patients to test medical students and graduates on their ability to gather information from patients, perform physical examinations, and communicate their findings to patients and colleagues.
Other Step 2 CS Resources
What To Bring (& What Not To Bring)
Important: If you do not bring acceptable identification, you will not be admitted to the test. In that event, you must pay a fee to reschedule your test. Your rescheduled test date(s) must fall within your assigned eligibility period.
On the day of your examination you must bring:
- The Scheduling Permit you received when your registration was completed
- Your Confirmation Notice
- An unexpired, government-issued form of identification that includes a photograph and signature. (i.e current driver's license or passport)
- Lab coat and stethoscope (not required, but strongly recommended, as there will be a limited supply available at the test center)
Each test center contains locked storage. You will be able to place personal items that you might need during breaks or during the exam at your seat in the orientation room. Luggage may not be stored in the center. There are no waiting facilities for spouses, family, or friends; plan to meet them elsewhere after the examination.
*Your name as it appears on your Scheduling Permit must match the name on your form(s) of identification exactly. The only acceptable differences are variations in capitalization; the presence of a middle name, middle initial, or suffix on one document and its absence on the other; or the presence of a middle name on one and middle initial on the other.
Please bring only necessary personal items with you to the center. You may not possess pens, cellular telephones, watches of any type, pagers, personal digital assistants (PDAs), two-way communication devices, or notes or study materials of any kind at any time during the examination, including during breaks. These items must be stored during the examination.
If you have a medical need for an item during your USMLE administration, a list of approved personal items is available.
Bulletin: Testing contains more information about the rules and regulations during the test.
What to Wear & When To Arrive
Wear comfortable, professional clothing and a white laboratory or clinic coat. The proctors will cover with adhesive tape anything on the laboratory coat that identifies either you or your institution.
- All examinees will be required to remove eyeglasses for visual inspection by the test center administrators. These inspections will be brief and will be performed during the check-in process.
- Jewelry, except for wedding and engagement rings, is prohibited.
- Hair accessories and neck ties are subject to inspection. Examinees should not wear ornate clips, combs, barrettes, headbands, and other hair accessories. Examinees wearing any of these items on test day may be asked to store such items in their locker.
The time you should arrive at the test center is listed in the Confirmation Notice you will print after scheduling your appointment.
Proper Behavior - Testing Regulations and Rules of Conduct
You cannot discuss the cases with your fellow examinees, during breaks or at any time.
Conversation among examinees in languages other than English about any subject is strictly prohibited at all times, including during breaks. Test center staff will be with you to monitor activity. To maintain security and quality assurance, each examination room is equipped with video cameras and microphones to record every patient encounter.
The USMLE program retains the right to remove any examinee from the examination who appears to represent a health or safety risk to the standardized patients or staff of a clinical skills evaluation center. This includes, but is not limited to, examinees who appear ill, are persistently coughing or sneezing, have open skin lesions, or have evidence of active bleeding. Examinees who are not feeling well are encouraged to seek medical advice prior to arrival at the center and, if consistent with medical advice, should consider rescheduling the date of their examination. This can be done at the website of your registration entity.
Clinical skills evaluation center staff monitor all testing administrations for the Step 2 CS examination. You must follow instructions of test center staff throughout the examination. Failure to do so may result in a determination of irregular behavior. The USMLE Bulletin of Information provides a complete description of irregular behavior and the consequences of a finding of irregular behavior.
Irregular Behavior:
Irregular behavior includes any action by applicants, examinees, potential applicants, or others when solicited by an applicant and/or examinee that could compromise the validity, integrity, or security of the USMLE examination process.
1. On-Site Orientation
Each examination session begins with an on-site orientation. If you arrive during the on-site orientation, you may be allowed to test; however, you will be required to sign a Late Admission Form. If you arrive after the on-site orientation, you will not be allowed to test. You will have to reschedule your testing appointment and will be required to pay the rescheduling fee.
*The clinical skills evaluation centers are secured facilities. Once you enter the secured area of the center for orientation, you may not leave that area until the examination is complete.
2. The Patient Encounter
Your Step 2 CS administration will include twelve patient encounters. These include a very small number of nonscored patient encounters, which are added for pilot testing new cases and other research purposes. Such cases are not counted in determining your score. You will have 15 minutes for each.
Announcements will tell you when to begin the patient encounter, when there are 5 minutes remaining, and when the patient encounter is over. In some cases you may complete the patient encounter in fewer than 15 minutes. If so, you may leave the examination room early, but you are not permitted to re-enter. Be certain that you have obtained all necessary information before leaving the examination room. Re-entering an examination room after leaving will be considered misconduct. Continuing to engage the patient after the announcement to stop has been made may be considered irregular behavior, will be reported to the USMLE, and could jeopardize your continued participation in the USMLE program.
If you are unsuccessful at Step 2 CS and must, therefore, repeat the examination, it is possible that during your repeat examination you will see similarities to cases or patients that you encountered on your prior attempt. Do not assume that the underlying problems are the same or that the encounter will unfold in exactly the same way. It is best if you approach each encounter, whether it seems familiar or not, with an open mind, responding appropriately to the information provided, the history gathered, and the results of the physical examination.
The Standardized Patient & Physical Examination
You should perform physical examination maneuvers correctly and expect that there will be positive physical findings in some instances. Some may be simulated, but you should accept them as real and factor them into your evolving differential diagnoses.
You should attend to appropriate hygiene and to patient comfort and modesty, as you would in the care of real patients. Female patients will be wearing bras, which you may ask them to loosen or move if necessary for a proper examination.
With real patients in a normal clinical setting, it is possible to obtain meaningful information during your physical examination without being unnecessarily forceful in palpating, percussing, or carrying out other maneuvers that involve touching. Your approach to examining standardized patients should be no different. Standardized patients are subjected to repeated physical examinations during the Step 2 CS exam; it is critical that you apply no more than the amount of pressure that is appropriate during maneuvers such as abdominal examination, examination of the gall bladder and liver, eliciting CVA tenderness, examination of the ears with an otoscope, and examination of the throat with a tongue depressor.
When you enter the room, you will usually encounter a standardized patient (if not, you will be asked to communicate with a standardized patient over the telephone). By relating to the patient in a patient-centered manner, asking relevant questions, and performing a focused physical examination, you will be able to gather enough information to develop a preliminary differential diagnosis and a diagnostic work-up plan, as well as begin to develop an effective physician-patient relationship.
Regardless of your current clinical role, during the patient encounter your expected role is that of at least a first-year postgraduate resident physician with primary responsibility for the care of each patient. You should treat each patient you see as you would a real patient. Communicate in a professional and empathetic manner, being responsive to the patient’s needs. Do not defer decision-making to others. It may be helpful to think of yourself working in a setting where you are the only provider present.
As you would when encountering real patients, respond appropriately to the patients’ needs for information exchange and understanding and engage them in planning for next steps.
Introduce yourself as you would in a professional setting. Do not mention the name of your school or institution.
The information you need to obtain in each encounter will be determined by the nature of the patient’s problems. Your approach should be focused. You will not have time to do a complete history and physical examination, nor will it be necessary to do so. Pursue the relevant parts of the examination, based on the patient’s problems and other information you learn during the encounter.
You should interact with the standardized patients as you would with any patients you may see with similar problems. The only exception is that certain parts of the physical examination must not be done: rectal, pelvic, genitourinary, inguinal hernia, female breast, or corneal reflex examinations. If you believe one or more of these examinations are indicated, you should include them in your proposed diagnostic work-up. All other examination maneuvers are completely acceptable, including femoral pulse exam, inguinal node exam, back exam, and axillary exam.
Another exception is that you should not swab the standardized patient's throat for a throat culture. If you believe that this diagnostic/laboratory test is indicated, include it on your proposed diagnostic workup.
Synthetic models, mannequins, or simulators provide an appropriate format for assessment of sensitive examination skills such as genital or rectal examination. Specific instructions will be provided in cases where this is necessary.
Excluding the restricted physical examination maneuvers, you should assume that you have consent to do a physical examination on all standardized patients, unless you are explicitly told not to do so as part of the examinee instructions for that case.
The cases are developed to present in a manner that simulates how patients present in real clinical settings. Therefore, most cases are designed realistically to present more than one diagnostic possibility. Based on the patient's presenting complaint and the additional information you obtain as you begin taking the history, you should consider all possible diagnoses and explore the relevant ones as time permits.
Telephone Patient Encounters
Telephone patient encounters begin like all encounters; you will read a doorway instruction sheet that provides specific information about the patient. As with all patient encounters, as soon as you hear the announcement that the encounter has begun, you may make notes about the case before entering the examination room.
When you enter the room, sit at the desk in front of the telephone.
- Do not dial any numbers.
- To place the call, press the yellow speaker button.
- You will be permitted to make only one phone call.
- Do not touch any buttons on the phone until you are ready to end the call - touching any buttons may disconnect you.
- To end the call, press the yellow speaker button.
- You will not be allowed to call back after you end the call.
Obviously, physical examination of the patient is not possible for telephone encounters, and will not be required. However, for these cases, as for all others, you will have relevant information and instructions and will be able to take a history and ask questions. As with other cases, you will write a patient note after the encounter. Because no physical examination is possible for telephone cases, leave that section of the patient note blank.
3. The Patient Note
Immediately after each patient encounter, you will have 10 minutes to complete a patient note. If you leave the patient encounter early, you may use the additional time for the note. You will be asked to type (on a computer) a patient note similar to the medical record you would compose after seeing a patient in a clinic, office, or emergency department. Examinees will not be permitted to handwrite the note, unless technical difficulties on the test day make the patient note typing program unavailable.
The ratings for the patient note are overseen by practicing physicians.
You should record pertinent medical history and physical examination findings obtained during the encounter, as well as your initial differential diagnoses (maximum of three). The diagnoses should be listed in order of likelihood. You should also indicate the pertinent positive and negative findings obtained from the history and physical examination to support each potential diagnosis.
While it is important that a physician be able to recognize findings that rule out certain serious or life-threatening diagnoses, the task for Step 2 CS examinees is to record only the most likely diagnoses, along with findings (positive and negative) that support them.
Finally, you will list the diagnostic studies you would order next for that particular patient. If you think a rectal, pelvic, inguinal hernia, genitourinary, female breast, or corneal reflex examination, or a throat swab, would have been indicated in the encounter, list it as part of the diagnostic studies. Treatment, consultations, or referrals should not be included.
A program for practicing typing the patient note is available in the Practice Materials
Calendar of Test Dates
Applicants registered for Step 2 CS can use the Step 2 CS Calendar and Scheduling system, available at the website of their registration entity (listed below), to check available test dates at the five Clinical Skills Evaluation Centers. This calendar is updated continuously to reflect applicant scheduling, rescheduling, and the opening of additional test dates, based on demand.
If you are interested in taking Step 2 CS, you are strongly encouraged to use the Step 2 CS calendar to monitor the availability of test dates. The only way to ensure a test date is to complete registration and scheduling through the Step 2 CS Calendar and Scheduling system.
NBME
For students / graduates of LCME-or AOA-accredited medical programs in the US or Canada:
ECFMG
For students / graduates of medical schools located outside the US and Canada:
If you are registered for Step 2 CS, please be aware that:
- The Step 2 CS scheduling system does not allow an applicant to reserve his/her scheduled testing appointment for another applicant, nor does it allow the transfer of a testing appointment from one applicant to another. When an applicant cancels a scheduled appointment, the appointment returns to the pool of available testing appointments where it can be claimed by other registrants.
- At any given time, many applicants registered for Step 2 CS may be attempting to schedule or reschedule testing appointments. It is common for appointments that become available to be claimed immediately by another applicant.
- The Step 2 CS scheduling system allows registered applicants to indicate their preferences for test dates and centers. When a testing appointment is canceled, all applicants participating in the email notification system who have expressed a preference for this date/center are notified immediately by email.
If you have any questions about the application process, you may fill out our Contact Form »
Scoring the Step 2 CS Exam
Step 2 CS is designed to evaluate your ability to gather information that is important for a given patient presentation. During your physical examination of the standardized patient, you should attempt to elicit important positive and negative signs. Make sure you engage the patient in discussion of your initial diagnostic impression and the diagnostic studies you will order.
The patients may ask questions, and you will see a range of personalities and styles in asking questions and presenting information. You should address each patient's concern as you would in a normal clinical setting.
The ability to communicate effectively with patients, demonstrating appropriate interpersonal skills, is essential to safe and effective patient care. Step 2 CS is intended to determine whether physicians seeking an initial license to practice medicine in the United States, regardless of country of origin, can communicate effectively with patients. The standardized patients assess communication skills, interpersonal skills, and English-speaking skills via carefully developed rating scales on which the standardized patients (SPs) have received intensive training.

On the patient note, your ability to document the findings from the patient encounter, diagnostic impression, and initial diagnostic studies will be rated by physician raters. You will be rated based upon the quality of documentation of important positive and negative findings from the history and physical examination, as well as the differential diagnoses, justification of those diagnoses, and diagnostic assessment plans that you list. As is the case with other aspects of Step 2 CS scoring, physician raters receive intensive training and monitoring to ensure consistency and fairness in rating.
Scoring the Subcomponents

USMLE Step 2 CS is a pass/fail examination.
Examinees are scored on three separate subcomponents: Communication and Interpersonal Skills (CIS), Spoken English Proficiency (SEP), and Integrated Clinical Encounter (ICE). Each of the three subcomponents must be passed in a single administration in order to achieve a passing performance on Step 2 CS.
The CIS subcomponent includes assessment of the patient-centered communication skills of fostering the relationship, gathering information, providing information, helping the patient make decisions, and supporting emotions. CIS performance is assessed by the standardized patients, who record these skills using a checklist based on observable behaviors.
Examinees demonstrate the ability to foster the relationship by listening attentively, showing interest in the patient as a person, and by demonstrating genuineness, caring, concern, and respect.
Examinees demonstrate skills in gathering information by using open-ended techniques that encourage the patient to explain the situation in his/her own words and in a manner relevant to the situation at hand, and by developing an understanding of the expectations and priorities of the patient and/or how the health issue has affected the patient.
Examinees demonstrate skills in providing information by using terms the patient can understand and by providing reasons that the patient can accept. These statements need to be clear and understandable and the words need to be those in common usage. The amount of information provided needs to be matched to the patient’s need, preference, and ability. The patient should be encouraged to develop and demonstrate a full and accurate understanding of key messages.
Examinees demonstrate helping the patient make decisions by outlining what should happen next, linked to a rationale, and by assessing a patient’s level of agreement, willingness, and ability to carry out next steps.
Examinees demonstrate the ability to support emotions when a clinical situation warrants it by seeking clarification or elaboration of the patient’s feelings and by using statements of understanding and support.
The SEP subcomponent includes assessment of clarity of spoken English communication within the context of the doctor-patient encounter (for example, pronunciation, word choice, and minimizing the need to repeat questions or statements). SEP performance is assessed by the standardized patients using a global rating scale, where the rating is based upon the frequency of pronunciation or word choice errors that affect comprehension and the amount of listener effort required to understand the examinee's questions and responses.
The ICE subcomponent includes assessments of both data gathering and data interpretation skills. Scoring for this subcomponent consists of a checklist completed by the standardized patients for the physical examination portion of the encounter, and global ratings for the patient note. Ratings for the patient note are overseen by practicing physicians. Patient notes are rated on the documented summary of the findings of the patient encounter (history and physical examination), diagnostic impressions, justification of the potential diagnoses, and initial patient diagnostic studies.
Copies of the patient note template, sample patient note styles, and software to practice typing the note are available in the practice materials. Although it is not feasible to list every action that might affect an examinee’s patient note score, the descriptions below are meant to serve as examples of actions that would add to or subtract from the score.
Cs Slotbola88
The following are examples of actions that would result in higher scores on the patient note:
- Using correct medical terminology
- Providing detailed documentation of pertinent history and physical findings. For example: writing “pharynx without exudate or erythema” is preferable to stating that the pharynx is clear.
- Listing only diagnoses supported by the history and findings (even if this is fewer than three)
- Listing the correct diagnoses in the order of likelihood, with the most likely diagnosis first
- Supporting diagnoses with pertinent findings obtained from the history and physical examination
The following are examples of actions that would result in lower scores on the patient note:
- Using inexact, nonmedical terminology, such as pulled muscle
- Listing improbable diagnoses with no supporting evidence
- Listing an appropriate diagnosis without listing supporting evidence
- Listing diagnoses without regard to the order of likelihood
Score Reporting Schedule
Csi Slots App
2020 Reporting Schedule - Step 2 CS
Calendar released April 1, 2019
| Testing Period | Reporting Start Date | Reporting End Date |
|---|---|---|
| January 1 - January 25 | March 4 | March 25 |
| January 26 - March 28 | April 29 | May 27 |
| March 29 - May 23* | June 24 | July 22 |
| May 24 - July 18 | August 19 | September 16 |
| July 19 - September 12 | October 14 | November 11 |
| September 13 - November 7 | December 16 | January 13, 2021 |
| November 8 - December 31 | February 3, 2021 | February 24, 2021 |
*No Step 2 CS exams will be delivered March 27 through April 4.
Slot Cs 1.6
Note: In each scoring cohort there will be occasional dates when individual test centers or the entire testing network are unavailable. These are typically known in advance, and the dates will be displayed as unavailable when examinees schedule appointments.
For each 'Testing Period' in the above schedule, Step 2 CS scores are released every Wednesday over a corresponding four-to five-week 'Reporting Period.' It is expected that results for the vast majority of examinees who take the exam during the testing period will be reported on the first Wednesday of the Reporting Period. Results for 98%-99% of examinees who take the exam during the testing period are reported by the third Wednesday in a Reporting Period. For a small percentage of examinees (1%-2%), scoring and quality assurance may be not completed in time for these examinees to be reported by the first three reporting dates; these will typically be examinees who took the exam in the latter part of the testing period. Results for these examinees will be reported each week throughout the reporting period, and should be reported no later than the last day of the score reporting period.
This schedule allows USMLE staff to enhance the quality assurance and data collection/scoring procedures performed prior to score reporting. Additionally, it provides examinees, as well as others who rely on Step 2 CS results, with guidelines regarding when a result will be reported for a given exam date. These guidelines allow examinees to plan their exam registration and scheduling in order to have their results in time to meet specific deadlines, such as those related to graduation or participation in the National Resident Matching Program (NRMP), or 'the Match.'
- Product lines
| Models with restrictor | ||||||
| Flow rate | Colour code | M16.5x1 (TT) | M18.5x1 (TJ) | M21.5x1 (JR) | M24x1 (STD) | |
|---|---|---|---|---|---|---|
| Z | 7.5 - 9.0 l/min at 3 bar | light green | – | 43.2202.450 | 42.2202.450 | 40.2202.450 |
| A | 13.5 - 15.0 l/min at 3 bar | light blue | – | 43.2203.450 | 42.2203.450 | 40.2203.450 |
| B | 22.8 - 25.2 l/min at 3 bar | dark blue | – | 43.2205.450 | 42.2205.450 | 40.2205.450 |
| C | 27.0 - 30.0 l/min at 3 bar | dark grey | – | – | – | 40.2206.450 |
| D | 34.8 - 37.8 l/min at 3 bar | light grey | – | – | – | 40.2207.450 |
| 1.0 gpm max at 60 psi | ivory | 44.3231.450 | – | – | 40.3231.450 | |
| T | 1.5 gpm max at 60 psi | green | 44.3232.450 | – | 42.3232.450 | 40.3232.450 |
| X | 2.2 gpm max at 60 psi | red | 44.3234.450 | 43.2201.450 | 42.2201.450 | 40.2201.450 |
| V | optimal performance and aeration from 0.2 to 1 bar | blue | 44.3230.450 | 43.3230.450 | 42.3230.450 | 40.3230.450 |
| PCA® models | ||||||
| Flow rate | Colour code | M16.5x1 (TT) | M18.5x1 (TJ) | M21.5x1 (JR) | M24x1 (STD) | |
|---|---|---|---|---|---|---|
| 0.5 gpm max. | lime | – | 43.2259.450 | 42.2278.450 | – | |
| 1.0 gpm max. | blue | 44.3258.450 | – | – | 40.2258.450 | |
| 1.2 gpm max. | pink | 44.3260.450 | – | – | 40.2260.450 | |
| 5.0 l/min | orange | 44.3251.450 | 43.2251.450 | 42.2251.450 | 40.2251.450 | |
| 1.5 gpm max. | green | 44.3256.450 | 43.2256.450 | 42.2256.450 | 40.2256.450 | |
| 6.0 l/min | black | – | – | – | 40.2252.450 | |
| 1.75 gpm max. | light blue | 44.3261.450 | 43.2261.450 | 42.2261.450 | 40.2261.450 | |
| 7.0 l/min | light green | 44.3255.450 | 43.2255.450 | 42.2255.450 | 40.2255.450 | |
| 2.0 gpm max. | lilac | 44.3257.450 | 43.2257.450 | 42.2257.450 | 40.2257.450 | |
| 2.2 gpm max. | yellow | 44.3253.450 | 43.2253.450 | 42.2253.450 | 40.2253.450 | |
| 8.0 l/min | white | 44.3254.450 | 43.2254.450 | 42.2254.450 | 40.2254.450 | |